Urologists from the Klinikum Oldenburg and scientists from the Faculty of Medicine are conducting joint research in the field of prostate cancer – with visible international success. Friedhelm Wawroschek, senior consultant at the Klinikum Oldenburg and Associate Dean for Clinical Affairs, is leading the research. As an expert in urological surgery and medical tumour therapy he sees enormous potential in the collaboration – from which patients stand to benefit.
“If you see a urologist run for your life!” The physician and surgeon Julius Hackethal made headlines with this piece of advice in 1978, sparking a medical controversy and causing huge anxiety among sufferers. He died in 1997 – from the effects of prostate cancer. His arguments about over-treatment, mutilation and “pet cancer” resonate to this day and are still discussed in expert circles. “Nobody dies of prostate cancer anymore”, is a statement Prof. Dr. Friedhelm Wawroschek still hears when he has to confront patients with a cancer diagnosis. But the numbers tell a different story. According to estimates by the Robert-Koch Institute in Berlin every year 65,000 men in Germany develop a malignant tumour of the prostate gland – and 12,000 of them die. The annual road death statistics, some 3,100 women, men and children, are significantly lower, although much more present in the collective consciousness. In fact, prostate cancer continues to be the most common form of cancer and the second most common cause of death from cancer for men in Germany.
Catch it early and nip it in the bud
“The prognosis is very good if the disease is detected early enough,” says Wawroschek, who has been the director of the University Hospital for Urology at the Klinikum Oldenburg since 2004. Since 2009 the senior consultant has run the German Cancer Society-certified Prostate Cancer Center Oldenburg at the Klinikum; he has been Professor of Urology at the University of Oldenburg School of Medicine and Health Sciences since June 2017, and Associate Dean for Medical Affairs since 2018. “What I like about my job is the variety,” the 54-year-old says, commenting on his extensive clinical and university activities. Even after over twenty-five years of professional experience he still enjoys working regularly in the operating room, although as head of the clinic he also has to deal with a lot of administration. For years now he has continued to develop prostate carcinoma research and the closely associated lymph node surgery at the Klinikum: “Diagnosis and therapy would not be where they are today otherwise.”
Wawroschek welcomes the interlinking of university-driven basic research and clinical research in Oldenburg: “Thanks to the research possibilities at the University we have been able to significantly professionalise in particular our clinical role in the field of lymph node surgery.” Additional funding and staff have helped establish good quality basic research with a high level of applicability, he adds.
Internationally visible research – in action
Since Wawroschek’s work amounts to more than a full-time job, he has handed over the supervision of research activities to his colleague PD Dr. Alexander Winter. The two physicians have known one another for almost two decades and already worked closely together during their time at the Klinikum Augsburg. Winter is a consultant, the acting head of the Prostate Cancer Center Oldenburg, and teaches at the University. The research findings he presents at national and international congresses stem from collaboration with the University, the associated OFFIS - Institute for Information Technology, the Klinikum Oldenburg and the Cancer Registry of Lower Saxony. In addition to improving diagnostics for lymph node surgery, Winter’s and Wawroschek’s speciality, these findings also address the realities of care – such as the current situation in the area of early detection – as well as future care needs.
In the meantime Winter’s research has garnered much international attention and recognition. One example is a new technology that makes it possible to mark sentinel lymph nodes in prostate cancer using superparamagnetic iron oxide nanoparticles. “These are minute particle that we use as an alternative to the usual radioactive labelling,” Winter explains. Why? An organ’s lymphatic fluid flows through the lymph nodes. If there is a malignant tumour in the prostate, sentinel lymph notes are the first filter station for the cancer cells. So surgeons need to know the exact location of these lymph nodes if they are to remove them or detect metastases. “This is why we have to mark them – either with a radioactively marked material or using our nanoparticles,” Winter continues.
“By implication I can surmise from the absence of tumours in the sentinel lymph node that lymphogenic metastasis is very unlikely to have occurred up to this point. In terms of therapy this makes it unnecessary to remove any further lymph nodes,” adds Wawroschek. The advantage of the new procedure, he says, is that the lymph drainage area of each individual patient can be taken into account, which results in comparatively few lymph nodes having to be removed – and thus in fewer complications. “The level of precision of our new magnetic method is comparable with the already established method, but magnetic marking does not involve exposing patients or staff to radiation,” Wawroschek says. Another advantage is that there is no longer any need for the expensive nuclear medicine infrastructure and its strict legal regulations. “This means magnetic marking is simple and uncomplicated for all urologists to use, which makes this method also interesting for countries with less sophisticated medical technology.
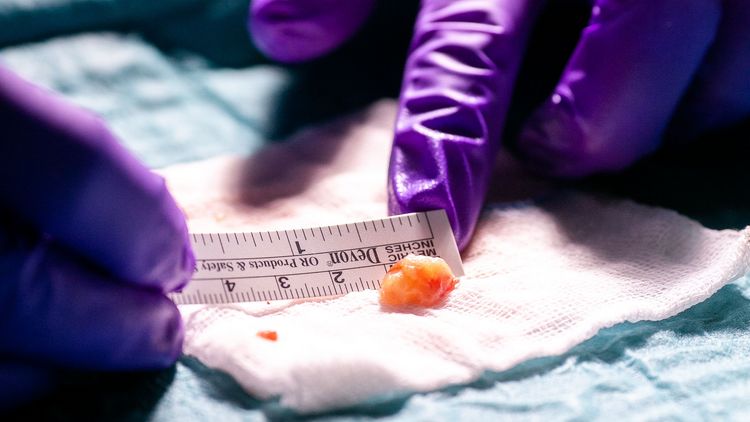
Once the surgeons have removed the marked lymph nodes, the work of the pathologist begins. They examine the lymphatic tissue for metastases, fixing, colouring and dissecting it. “There is no standardisation for this procedure though,” Wawroschek explains. In simplified terms this means that if you don’t look closely enough or you take too few sections from the lymph nodes you could overlook small or micrometastases. “However thorough the pathologist’s work, there is always a minimal, residual risk of missing something,” Wawroschek says. The only way around this would be to come up with a method that examines the lymph node right down to the level of its molecular genetic components. “That’s our next project, and we have already carried out a promising pilot study for it at the Klinikum,” Winter explains.
An Innovative molecular detection method
In the summer of 2018 Winter presented this project involving a new molecular procedure for detecting lymph node metastases in prostate cancer - the first of its kind worldwide - at the annual meeting of the American Urological Association in San Francisco. Developed in collaboration with pathologists, the so-called “OSNA analysis” (one-step nucleic acid amplification) attracted a high level of interest among urological experts and was named the best contribution in this subject area. “This novel method has significant clinical relevance. And unlike many other good approaches, its implementation is within reach,” Winter explains.
The idea behind it: A largely automated molecular genetic procedure seeks out the RNA messenger of a particular protein in the lymph node, Cytokeratin 19 (CK19), which is present in the prostate but normally not in the lymph nodes. “We can even determine the amount of CK19 in the lymph nodes – and this all could takes place in the operating room” Winter emphasises. The lymph node can be completely analysed within 30 to 40 minutes – then we have an unambiguous result, with no risk of human misdiagnosis. “We can get the results during the operation and if necessary extend the lymph node dissection or adapt the subsequent therapy,” Wawroschek adds. This saves the patient from having to wait for results after their operation and could even spare them further operations or additional radiation treatment.
The Oldenburg researchers are convinced that the method can be established as a standard procedure for lymph nodes. “OSNA analysis still needs to be validated, and we’re working on that,” Wawroschek says. Both the magnetic marking of sentinel lymph nodes and the detection of lymph node metastases are examples of how the still very fresh collaboration between clinical and university research is already yielding important fruits. Wawroschek and Winter see enormous potential in this joint research for future developments in their field. “Each person brings their own expertise to the table, and together we expand our horizons – all in the name of providing better treatment for patients.”