New insights are paving the way for highly targeted cancer therapies. In this interview, Frank Griesinger, director of the Centre for Internal Medicine – Oncology at Oldenburg Pius Hospital, explains the latest results of a clinical trial.
Professor Griesinger, in clinical studies you are studying the use of targeted drugs to treat certain forms of lung cancer that result from a known gene mutation. What is special about this approach?
All cancers are based on one or several gene mutations – in other words changes in the genetic make-up of a cell that turn a healthy cell into a malignant one. We call these cells oncogenes. Many such mutations are now well-known, for example the so-called KRAS mutation, which plays a role in many types of cancer. Great advances are being made in the development of drugs that target these mutations, particularly when it comes to lung cancer. Due to their efficacy and good tolerability these drugs offer several advantages over chemotherapy, a far less targeted form of therapy.
The results of a clinical study in which you were involved were recently published in “The New England Journal of Medicine”. What was the study about?
We are involved in the clinical research on a new drug called Tepotinib. This drug helps patients with a specific gene mutation. The mutation is found in three to four percent of all patients with non-small cell lung cancer, the most common form of lung cancer. That’s about 1,000 to 1,200 people in Germany every year. This gene mutation - we experts call it a MET exon 14 skipping mutation – blocks the breakdown of a certain protein in the cell. The protein then accumulates in the cell and contributes to its transformation into a tumour cell, because the mutation switches off a waste disposal signal which normally regulates the breakdown of the protein. The new drug Tepotinib inhibits the signalling pathway of the excess protein and thus triggers the death of the cancer cell.
How did you come to be involved in this international study?
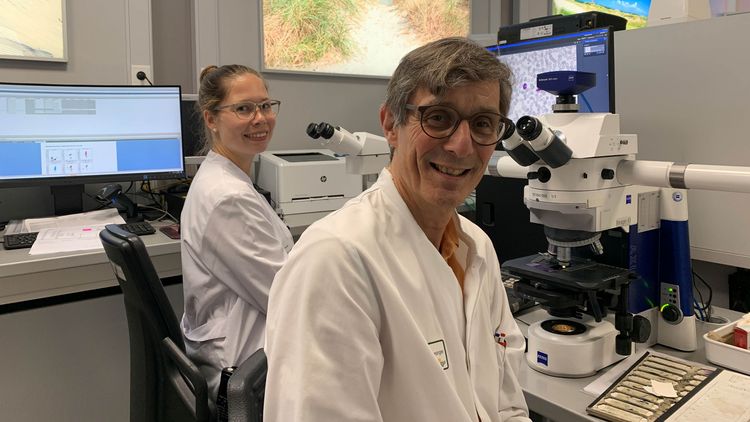
Together with my colleagues from the Institute for Haematopathology Hamburg, Professor Lukas Heukamp and Professor Markus Tiemann, we built up the NOWEL network. Through this network we receive tissue samples from patients with lung cancer and use a complicated procedure to test them for genetic mutations. Our work in this network also enables us to offer patients innovative drugs in the context of clinical studies. This makes us an attractive option for patients from other regions in Germany who come to us for treatment. Patients with rare diseases are particularly eager to take advantage of such opportunities. As a university institution, we enjoy a higher degree of visibility, which makes us an attractive choice for carrying out clinical studies.
What are the most important results of the recently published study?
A total of 152 patients worldwide took part in the study, 99 of whom we monitored for at least nine months. Eight patients from Oldenburg were included. We conducted a so-called phase II study. This means that the patients were given the new drug without it being compared to a standard therapy, for example chemotherapy. The aim was to test whether patients with the mutation responded to the drug. This was the case in 50 to 60 percent of the patients - regardless of previous therapies. That’s an encouraging result. The therapy is also very well tolerated – apart from some cases of oedema, which can affect the legs and arms and is sometimes not easy to treat.
What other advantages do these targeted therapies offer?
The patients only need to take pills – which is of course far easier than administering chemotherapy. The good thing is that patients aren’t so restricted during the therapy. Some feel fit enough to lead a completely normal life – even now, during the Covid-19 pandemic. Of course, they are probably at a slightly higher risk due to the cancer. But many of them can still work and take part in everyday life and keep up their social life.
But the study is also significant for another reason…
Yes. Sometimes the tissue we receive from patients is insufficient to carry out tests for genetic mutations. So we try to find evidence of genetic mutation of the tumour using a “liquid biopsy”. In this study, for the first time we were able to identify patients solely on the basis of the genetic mutation detected via liquid biopsy, and then include them in the therapy. We developed this diagnostic procedure together with our colleagues from Hamburg and carry it out at the Pius Hospital. We were able to demonstrate that this method of detection is just as good as testing tumour tissue.
So what comes next?
Until now it has only been possible to use the drug in the context of the study. It is now in the accelerated approval programme of the US Food and Drug Administration (FDA). Later on it will hopefully be approved by the European Medicines Agency (EMA). In addition, Phase III clinical trials will be carried out to test whether patients respond better to this therapy than to standard therapies such as chemotherapy. We researchers here in Oldenburg will also be involved in these study concepts.
Interview: Constanze Böttcher