Research
Research
Research of the Department of Experimental Allergology and Immunodermatology
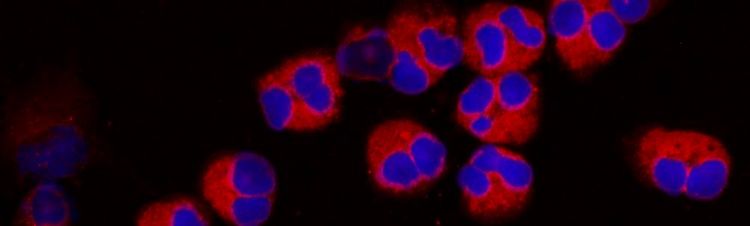
The focus of our research group is on autoimmune diseases such as bullous pemphigoid, allergies, skin cancer and inflammatory skin diseases including atopic dermatitis, contact eczema and psoriasis. We are particularly interested in the role of basophils and eosinophils in these diseases, as the inflammatory mediators released from these cells play a crucial role in the severity of symptoms and also act on other immune cells that control these diseases. Our group has many years of experience in isolating and purifying human allergic effector cells to study their functional responses and to elucidate the intracellular signalling mechanisms that control their reactivity. Our main goal is to understand the different roles of these cells in autoimmunity and allergy and to develop new therapeutic strategies.
Ongoing international research collaborations include the University of Groningen (NL), where we are investigating the causes of skin blistering in bullous pemphigoid and the role of TRP channels in atopic dermatitis. We are also a member of the translational PruSeach research group, which is funded by the German Research Foundation (DFG). In close co-operation with the Universities of Heidelberg, Düsseldorf, Münster, Mainz, Erlangen and Würzburg, we hope to unravel the novel mechanisms of itch and its link to pain and identify new treatment targets. Other cooperation partners are the University of Leuven (Belgium) and the Hannover Medical School, with whom we are researching fundamental questions about the role of inflammatory mediators in chronic inflammatory skin diseases.
Bullous pemphigoid
Bullous pemphigoid (BP) is a blistering autoimmune dermatosis that belongs to the group of rare autoimmune diseases. The symptoms of bullous pemphigoid are initially described by itching with erythema and later by the appearance of bulging blisters. Bullous pemphigoid mainly occurs in older people. The aetiology of bullous pemphigoid is explained by the formation of IgG autoantibodies to hemidesmosomal antigens such as bullous pemphigoid antigen 1 (BP230) and bullous pemphigoid antigen 2 (BP180). BP180 is a transmembrane member of the collagen protein type XVII that has been identified as the primary antigenic target of BP autoantibodies. BP180 is expressed on the basal surface of basal epidermal keratinocytes and is a member of the hemidesmosomal complex, a cellular structure that functions as a dermo-epidermal adhesion. The major epitopes of BP180 associated with the disease map to the NC16A domain. In addition to IgG auto-AK, IgE AK also play a pathogenetic role in bullous pemhpigoid.
A massive infiltrate of eosinophilic granulocytes is characteristic of bullous pemphigoid. The blistering is not only caused by the binding of auto-AK, but also by the mainly granulocytic infiltrate, complement and eosinophil proteases. In addition, the number of basophilic granulocytes in the dermis is increased in patients with bullous pemphigoid.
We are particularly interested in the role of basophilic and eosinophilic granulocytes in bullous pemphigoid. The research is funded by the DFG, among others. In addition, we have a research collaboration with Prof Dr Marcel Jonkman's group at UMCG Groningen, in which we are jointly investigating the causes of blistering of the skin in bullous pemphigoid as part of a Joint-Ph.D. programme(Project 4: "Bullous pemphigoid - What makes the blister?").
Chronic pruritus
Chronic pruritus ("chronic itching ") is one of the most common symptoms of many skin diseases and can significantly worsen the quality of life. Chronic inflammatory skin diseases, including lichen planus (LP), psoriasis (PSO) and atopic dermatitis (AD), are a major cause of chronic pruritus. Nevertheless, these diseases differ fundamentally in terms of phenotype, histopathology and immunological principles underlying disease progression. There is increasing evidence that IL-17, IL-31, NGF and TSLP play a crucial role in pruritus formation. Therapeutic antibodies targeting either IL-17A or IL-31A have been shown to effectively reduce pruritus in PSO and AD, respectively. However, the molecular basis of chronic pruritus in skin inflammation is still largely unclear.
Our main goal is to characterise known (IL-31, NGF, TSLP) and identify novel pruritus signalling pathways in chronic skin inflammation using transcriptome and cytokine analyses of skin-infiltrating T cells, mast cells and eosinophilic granulocytes, as well as peripheral blood mononuclear cells (PBMCs), in order to open up new therapeutic opportunities.
Our research group is part of the Translational Pruritus Research group (PruSearch FOR 2690), which is funded by the German Research Foundation (DFG). The research group consists of scientists and experts in the field of pruritus research in Germany with different areas of expertise such as dermatology, neurophysiology, anaesthesiology, neurology, gastroenterology and radiology. Within the framework of this research group, we are identifying and characterising pruritus signalling pathways in chronic skin inflammation together with the research group of Prof Dr Bernhard Homey from the UKD Düsseldorf (Project 5: Identification and characterisation of pruritus signalling pathways in chronic skin inflammation).
TRP channels
Atopic dermatitis (AD) is a chronic itchy and inflammatory skin disease that severely affects patients' quality of life. The mechanism of chronic itching in AD is not yet fully understood. Eosinophils and basophilic granulocytes are responsible for triggering and maintaining inflammation in atopic dermatitis. In this context, we have shown that a bidirectional interaction between eosinophils and peripheral nerves plays a role in AD pathology. There is growing evidence that TRP (Transient Receptor Potential) channels are involved in the mechanisms of neuro-immune interaction related to itch and inflammation. TRP channels are mainly expressed by sensory neurons, but recent studies have shown that they are also functionally expressed in immune cells, T cells and neutrophils. By maintaining intracellular calcium homeostasis, TRP channels regulate various functions of these cells, such as the release of itch-inducing and proinflammatory mediators, cell migration and cell death. The aim of this translational project is to characterise the expression and function of TRP channels.
The project is funded by the research pool of the School of Medicine and Public Health of the University of Oldenburg (Atopic Dermatitis - novel functions of TRP channels in neuro immune interaction mechanism; uol.de/medizin/forschungspool/uebersicht-gefoerderter-forschungspoolprojekte).
Role of IL-31/IL-31RA axis in human neutrophils in pruritic skin inflammation".
skin inflammation"
Atopic dermatitis (AD) is a chronic, itchy and inflammatory skin disease that severely affects patients' quality of life. The mechanisms of chronic itching and inflammation in atopic dermatitis are not yet fully understood. In general, itch is mediated by a complex interplay of inflammatory mediators, immune cells, skin cells and neuronal networks. Neutrophil granulocytes are responsible for triggering and maintaining inflammation in AD. A key mediator and link between immune cells and neurons in pruritus is the cytokine interleukin-31 (IL-31), which promotes neuron sprouting. IL-31 is secreted by various immune cells such as T cells, eosinophils and basophils and is signalled via a receptor complex consisting of the IL-31 receptor alpha (IL-31RA) and the oncostatin M receptor beta (OSMRβ). In this context, we detected the expression of IL-31 on eosinophils and basophils and the expression of the IL-31RA and OSMRβ receptors on basophils. The aim of this translational project is to investigate the expression and modulation of IL-31RA and OSMRβ and the functional role of IL-31 on neutrophils.
The project is funded by the Research Pool of the School of Medicine and Public Health of the University of Oldenburg ("Role of IL-31/IL-31RA axis in human neutrophils in pruritic skin inflammation") uol.de/medizin/forschungspool/uebersicht-gefoerderter-forschungspoolprojekte).
