Projects
Projects
CareFall
Cardiorespiratory fitness - influencing factor for fall risk and gait safety in older people?
Impaired static balance is a risk factor for falls in older people. Cross-sectional studies suggest a correlation between static balance and individual aerobic exertion. However, the influence of aerobic stress on dynamic balance has not yet been investigated and the influence of endurance capacity on the risk of falling or the rate of falls and dynamic balance is currently unclear.
The CareFall study uses an exploratory approach to investigate the potential relationship between individual endurance capacity and fall risk as measured by static and dynamic balance.
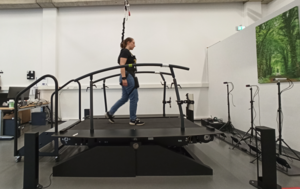
Endurance capacity is investigated by analyzing cardiovascular regulation in the moderate exercise range. Dynamic balance will be tested with a perturbation treadmill, which provokes standardized gait disturbances, before and after short phases of walking and compared between a group of people with a history of falls and a group without a history of falls.
Potentially, new intervention strategies can be developed on the basis of the CareFall project, as well as diagnostic options for use in everyday life.


Drop it
Blood pressure regulation when sitting and standing
In order to move safely from a lying position to a standing position, not only must sufficient muscle strength be available, but the blood pressure must also react appropriately. The change in position leads to a temporary redistribution of blood in the body. The body counteracts this redistribution through the so-called "orthostasis reaction", e.g. by increasing the heart rate.
A limited "orthostasis reaction" can lead to dizziness or, in particularly serious cases, to a brief loss of consciousness - i.e. syncope. It is not uncommon for these symptoms to lead to falls with serious injuries.
In a clinical context, it is important to record the functionality of the "orthostasis reaction" and to be able to improve it in a targeted manner if it is impaired. The regular test requires the patient to stand up. This is not always possible, especially during an inpatient stay, for example due to injuries. For this reason, the geriatric ward and the Geriatric Traumatology Center at Oldenburg Hospital are investigating whether the functionality of the orthostatic reaction can also be recorded during the transition from lying to sitting.
mGang
Mobile analysis and classification of gait and balance disorders

Project logo created by: Ms. Yvonne Feld, "Many thanks" from the entire geriatrics team.
An increased incidence of near-falls (such as trips, slips or missteps) and a worsening response to these events are associated with an increased risk of falling. Falls are one of the most common reasons for hospitalization and immobilization in old age. Early detection is very important in order to increase the success of preventive measures.
As part of the mGang project, we want to detect near-falls and the reaction to them and bring them from the high-tech professional laboratory into people's everyday lives. A mobile assessment outside the laboratory offers the prospect of greater availability, better mapping of everyday situations and additional diagnostic information. Gait data is recorded using professional laboratory equipment on the one hand and generally available devices such as smartphones and hearing aids on the other, and then compared. In order to simulate near falls as closely as possible under safe conditions, standardized disturbances are provoked with a perturbation treadmill while the test subjects are secured. In addition, the test subjects will each walk a 6 m long route on flat and uneven ground and undergo various geriatric tests.
In the long term, the valid recording of near-falls and the evaluation of the reaction to them will be carried out with the help of generally available mobile technology (smartphones, hearing aids).
The project is part of the interdisciplinary potential area of mobile health (mHealth) of the University of Oldenburg, the aim of which is to develop basic principles and prototype solutions for applications of mobile, digital health support via smartphone.


STRAHIL
Fear of falling in the course of geriatric rehabilitation: the perspective of patients and their relatives
As part of the "STRAHIL" project, we would like to investigate whether a possible fear of falling can be reduced by both patients and their relatives or loved ones through a geriatric rehabilitation program.
The study takes place during a stay at the Oldenburg rehabilitation center.
At the beginning and end of the stay, functional tests are carried out and patients are asked about their fear of falling. If possible, a person close to the patient is also asked about their fear of their relative falling. This survey is repeated three months after discharge.
This data will be used to analyze the extent to which the patient's perception coincides with that of the next of kin/caregiver and the extent to which the patient's fear of falling may be influenced by that of the next of kin or caregiver.
FriDA-F
Post-inpatient development of the ability to perform daily activities in elderly patients after fracture (broken bone) of the spine and pelvis
The study is being conducted as a multi-center study in Stuttgart, Oldenburg and Aachen . The Robert Bosch Hospital in Stuttgart is leading the study.
Spinal and pelvic fractures are frequently treated fractures in German hospitals. Compared to hip fractures, the cause of these two fractures has been little studied.
Data on quality of life, participation, need for assistance, functionality/mobility, pain and fear of falling are to be collected from patients after spinal and pelvic fractures following inpatient admission to Oldenburg Hospital . The aim of the study is to establish a cohort, including a biodatabase.
The FriDA-F study focuses on the following questions:
- What percentage of spinal and pelvic fractures can be attributed to falls?
- Which parts of the spine are particularly affected by falls?
- Which biomechanical fall sequences contribute to a vertebral or pelvic fracture?
- Which characteristics contribute positively and negatively to functionality, mobility, falls and/or impairment or participation in patients with vertebral or pelvic fractures?
- Development of an age trauma register for the vertebral body and pelvic fracture groups
- Establishment of a biodatabase to investigate the biological causes of abnormalities in the post-inpatient development of the ability to perform everyday activities in older patients following a fracture of the spine and pelvis. For example, bone-relevant biomarkers are to be determined and the bone status of the affected patients investigated. Other aspects, such as nutrition and/or medication intake, can have a significant influence on the post-inpatient development of the ability to perform everyday activities in older patients. Investigations, e.g. of drug concentrations, can help to better understand the causes of the development of patients' ability to perform daily activities after a vertebral body or pelvic fracture.
EDDY-PRO
Detection of age-dependent differences in dynamic balance during walking as fall protection
Correlations with functional parameters
Falls are a significant cost factor for the healthcare system. It is important to analyze the reasons for falls in order to prevent them through physical training or adjustments in daily life. One of the main factors for an increased risk of falling is reduced balance. Perturbations on a treadmill can be used to analyze the reactive dynamic balance that is often required in everyday life (slipperiness, approaching a bus). With the help of a perturbation treadmill, patients can be tested and trained in a standardized and repeatable manner under safe conditions.
To date, there has been a lack of studies on older people with a history of falls with regard to their dynamic reactive balance on a perturbation treadmill and a comparison with older or young healthy adults. Previous studies only aimed to compare older and younger healthy individuals. No significant differences were found between these groups.
The aim of the EDDY-PRO study is now to determine whether there are differences between a group of older people (70+) with a history of falls and older (70+) and younger (18-30 years) people who have not yet fallen.
The subjects will be asked about their medication intake and various other aspects of individual fall risk. Furthermore, functional tests are carried out with the participants and their static and dynamic reactive balance is recorded using a perturbation treadmill.
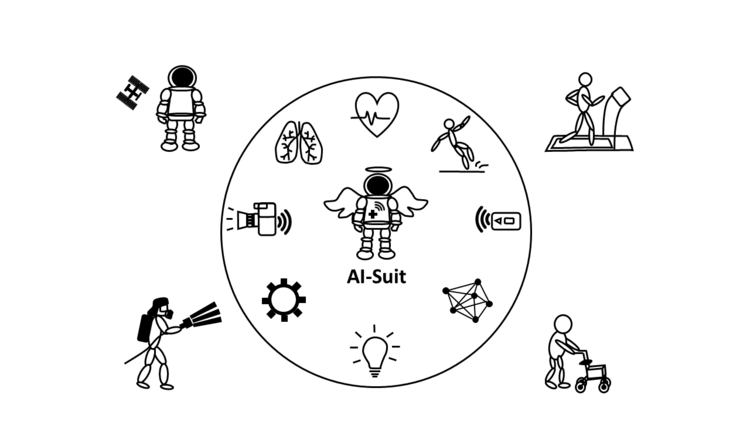
AI optimized space suit (AI suit)
Motivation
With the commercialization of space travel, the journey into space is becoming accessible to a wider audience. In the future, not only highly educated and highly trained space travelers will go into space. This will also change the demands on space suits and the health requirements.
In order to be medically and technically prepared for this situation, new technologies and measurement methods will be tested and adapted to the new conditions.
Approach & Goals
Protective suits for space travelers serve to safeguard vital functions during launch and landing as well as during missions in a vacuum. Today's suits are already equipped with various sensors, especially for temperature and oxygen concentration monitoring. The recording of vital parameters ranges from punctual measurements at specific points in time to continuous measurements. The sensor data is collected in the spacecraft and then sent to the ground station.
The goal of the overall AI-Suit project is to continuously record the stress level with the help of artificial intelligence (AI). In the future, critical health conditions will be detected at an early stage and selective feedback will be given to the space travelers. Since critical incidents are detected locally, contact to the base station and the amount of data transmitted will be reduced.
Concepts for a design of miniaturized, AI-based, yet energy-efficient sensing patches and their implementation/evaluation will be explored. The application is intended to realize optimized, digital health monitoring of the spacefarer:s and to provide preventive warning of immediate overload. For use in space, (e.g., blood pressure) as a vital parameter enables important statements about the effects of microgravity on the human blood circulation and, in combination with heart rate, is essential for determining the state of stress. The novel research approach of artificial intelligence is used for fast and efficient calculation of the data. The integration of expert knowledge ensures that the machine learning algorithms used are not a black box.
In parallel, we are investigating how the knowledge and tools gained can also be used in the medical field. One obvious example is the use of sensor technology for continuous monitoring in the clinical field.
Innovations in geriatric group therapy: feasibility and acceptance of square-stepping exercise and treadmill perturbation training in geriatric rehabilitation.
The Department of Geriatrics at the University of Oldenburg and the Klinikum Bremerhaven Reinkenheide, under the direction of Dr. Svenja Tietgen, are conducting a group intervention in geriatric inpatient (acute) rehabilitation at the Rehazentrum Oldenburg and the Klinikum Bremerhaven Reinkenheide to investigate the feasibility and acceptance of the so-called "Square-Stepping Exercise" and "treadmill-based perturbation training" (only in Oldenburg) in these settings.
The Square-Stepping Exercise involves walking and learning grid patterns on a carpet with 4x10 boxes. This training was developed in Japan for independently living older people to improve hip and leg strength and has been shown to improve brain performance, as well as learning to lunge after a tripping event, reducing the risk of falls.
The treadmill-based perturbation training, which is additionally carried out at the Rehazentrum Oldenburg on the Balance Tutor, can perturb your gait under safe conditions. The participants learn how to react to unexpected disturbances in their gait. During the training, the participants are secured by a belt system.
The aim is to define suitable participation criteria for the "Square Stepping Exercise" and the "treadmill-based perturbation training" for (acute) rehabilitation. In addition, we want to obtain information about the feasibility of the group format.
The subjective side of delirium (SSD)
The subjective side of delirium (SSD)
The explorative single-arm study is multicentre, carried out in co-operation with the Agaplesion Bethesda Hospital Bergedorf in Hamburg and the Bremerhaven Reinkenheide Hospital in Bremerhaven and includes both qualitative and quantitative aspects.
Delirium is a serious, acute state of confusion that often occurs in older people during a hospital stay. Little is known about the subjective side of delirium, i.e. the experiences of the person affected, except for individual case reports. Patients who have overcome delirium report very different perceptions, which have so far only been recorded in small studies. The interviews with patients who have experienced delirium should help to characterise the experience of those affected and help to identify starting points for delirium treatment as well as to analyse the connection between subjective experiences and objectifiable data.
ConVideo
Video-based physiotherapy in older adults in the context of the COVID-19 pandemic- "ConVideo".
Older people were considered as a high-risk group for a severe course of COVID-19 infections, and were therefore encouraged to limit their social life and their daily activities outside their own home as much as possible. However, reducing daily activities increases the risk to lose muscle strength and functional abilities. Although physiotherapy could be used to counteract these losses, many older patients avoid contact with physiotherapists in order to prevent infection.
During the pandemic, the health insurance associations at the national level and the GKV-Spitzenverband decided, to allow the conduction of physiotherapy via video. The possibility and willingness of older people to use this form of therapy and possible barriers are not yet known. The same applies to the technical and organizational framework for this therapy option.
The purpose of this study is to investigate whether and how the provision of video-based physiotherapy has an effect on the maintenance of care for persons aged 60 years and older and how the new form of therapy is subjectively perceived by physiotherapists and patients or which forms of therapy are or are not suitable for video therapy. Another goal is to assess activity, participation, and health-related quality of life before, during, and after the corona crisis or its associated limitations.
Participating physiotherapy practices in the Oldenburg area were supported by the study team in providing video therapy to individuals above the age of 60 years by providing hardware (tablets with mobile data) with appropriate software (video telephone application) and received instructions on how to use the system. At baseline and after completion of the study, sociodemographic and health-related data as well as standardized questionnaires on physical activity, quality of life, and participation were collected by means of telephone interviews to assess the impact of the corona crisis on patients. Therapists briefly document aspects of the connection quality and feasibility of the treatment after each therapy session. Patients were asked about their subjective perception of videotherapy after the end of the study.
RollGa
Effects of rollator use on posture, gait and balance in old age (RollGa)
The use of rollators is widespread and is intended to support safety when walking, the preservation of walking ability and the associated independence in old age. However, their use also carries risks of falls and an increasing loss of physiological gait. After initial improvements of the gait pattern, a deterioration of gait quality often occurs with continued rollator use. The effects of a rollator on posture in combination with dynamic balance have not yet been investigated.
In this study, the influence of a rollator on posture, physiological gait pattern and dynamic balance in older people aged 70 and over will be investigated. The project will be implemented using qualitative (Phase I) and quantitative methods (Phase II).
In phase I, individual interviews with rollator users and focus group discussions with medical professionals will be conducted. In this way, needs can be identified and an internal view of the prescription processes regarding rollator use can be analysed. In phase II of the project, gait analyses will be carried out on test persons with and without a rollator as well as persons with and without subjective gait insecurity. The measurements will be carried out using a new type of treadmill. Everyday disturbances in the gait pattern (e.g. stumbling or swaying) can thus be simulated under safe conditions and provide new insights into the movement behaviour of the different groups.
The aim is to implement the findings in the care process for people with gait disorders. This includes the development of standardised criteria for the indication of a rollator and the development of intervention programmes to improve the gait pattern and reduce the risk of falls in permanent and transitional rollator use.
CoNFINE
Constraints on social life in the context of the COVID-19 pandemic - impact on physical capacity and health-related quality of life of older people (CoNFINE)
The measures taken to flatten the infection rate during the Covid-19 pandemic were accompanied by enormous restrictions on social life, some of which still persist at present. In particular, the at-risk group of older people not only comply with the respective imposed contact bans, but have also been restricting their activities of daily living on their own for quite some time. Especially the two-month interruption of the availability of structured sports activities could have an enormous impact on the physical performance and health-related quality of life of older people and be more pronounced compared to younger people. To assess the impact of these limitations, the study will compare older (≥ 60 years) and younger (45-59 years) people from physiotherapy practices exercising in a milon circuit. The training data recorded via the milon circuit software allow an objective comparison of physical performance before the measures came into effect from mid-March with the training data that can be recorded when training is resumed. These values will be compared between age groups as well as followed up over a period of 6 months after resumption of training. Participants will be asked about their physical activity and quality of life before, during (retrospectively) and after the pandemic-related limitations. On the one hand, this enables the recording of objectively measurable functional changes and, on the other hand, the survey and comparison with possible changes in physical activity and quality of life during and after the limitations of social life and structured training opportunities in the context of the COVID-19 pandemic.
Reference care
Introduction of a care system for people with dementia
The project "Introduction of patient-centered care for people with dementia" was funded by the Lower Saxony State Office for Social Affairs, Youth and Family. Starting in 2020, a patient-centred care system was set up at the geriatric ward and in the geriatric trauma centre of the Klinikum Oldenburg. Care givers were trained to give individualized care for patients with dementia and or delirium, and worked outside of regular working shifts. The scientific part of the project was designed to observe the improvement of care for patients with dementia by nursing staff, as well as the overall perception of these specialized nursing staff by the team of the respective ward.
In this context, the potential improvement in delirium, depression, cognitive status, frequency of falls, eating behaviour, and length of hospital stay was documented. Functional and cognitive abilities as well as food intake were recorded before, during and at the end of the hospital stay. Family members were also surveyed to rate the patient-centred care system.
In addition, it was assessed how the nursing team in the hospital can be relieved by the specialized nursing staff who, for example, can no longer work in the 3-shift model for, i.e. family reasons.
MPI Covid-19
The Multidimensional Prognostic Index (MPI) for prognostic stratification of older hospitalised patients with Covid-19: a prospective observational cohort Study (MPI_Covid-19).
The study will investigate the applicability of the Multidimensional Prognostic Index (MPI) among hospitalised patients above the age of 65 years who are infected with COVID-19.
This observational, prospective, multicentre study is led by Prof. Priv.-Doz. Dr. Dr. M. Cristina Polidori Nelles of the Clinic II for Internal Medicine at the University of Cologne.
The MPI is a prognostic tool to determe short-term and long-term mortality risk. Multicentre studies have already shown that the MPI had excellent accuracy and calibration in predicting clinical outcomes during hospitalisation and its duration. To date, the MPI has been validated in over 50 international studies involving more than 54,000 older adults suffering from the most common chronic and acute age-related diseases associated with high mortality. Recently, it was demonstrated that the MPI can predict clinical outcome after non-invasive ventilation in patients with respiratory failure. Up to now, there are no studies on the use of the MPI to predict prognosis in older COVID-19 patients.
The MPI is calculated using information derived from a standardised comprehensive geriatric assessment in eight domains: basal and instrumental activities of daily living, cognitive status, risk of decubitus due to immobility, nutrition, multimorbidity, number of medications taken, living situation.
The primary objective of this study is to assess, if the MPI is able to predict 1) the ICU admission, and 2) the mortality in hospitals among older inpatients with a Covid-19 infection. Furthermore, it is assessed, if the MPI after three months can predict a) the duration of stay, b) rehospitalisation, c) admission to long-term care facilities, and/or d) mortality.

