The Studies
The Studies
The model course of study in human medicine was established in the winter semester 2012/13. A central objective of the study programme is to train students in all the competences required in the medical profession and to prepare them for the future profession from the very beginning through a patient-oriented study programme. The CanMEDS framework model forms the basis for this. The Oldenburg curriculum is characterised in particular by consistent modularisation and integrated, interdisciplinary, competence-based and patient-oriented training.
Studying in the model degree program at the CvO means:
- Practical orientation: Prospective doctors gain practical experience in courses, observation and internships from the first semester onwards.
- Interdisciplinary learning: Students acquire knowledge and skills across disciplines in integrated modules.
- Research orientation: The scientific training of medical students begins in the first year of study and continues as a longitudinal element (research pathway) throughout the entire study programme up to the PJ.
- Crossing borders: Students can spend up to two years of their studies at the Rijksuniversiteit Groningen.
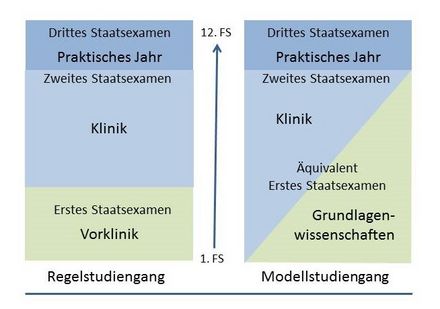
What is a model study programme?
The Oldenburg curriculum is characterised in particular by consistent modularisation and integrated, interdisciplinary, competence-based and patient-oriented training.
In contrast to standard degree programmes, which initially focus on teaching the basic sciences (preclinical), students in the model degree programme learn basic scientific and clinical content from day one. Under protected conditions, practical skills in the Clinical Training Centre as well as communication situations with actors are instructed and practised from the beginning. The students also have contact with patients from the first semester.
The curriculum
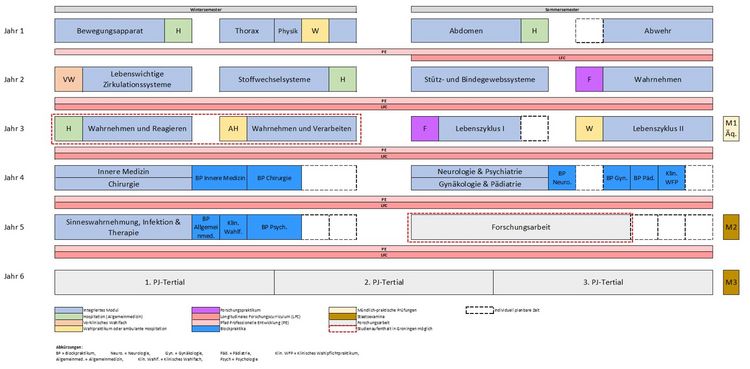
The curriculum in the model degree programme in human medicine is characterised by an exceptionally strong integration of patient and practice orientation in a spiral curriculum. The first three years of study are divided into four 10-week modules each, which are consistently structured in an interdisciplinary way. In the first year, mainly basics are taught; students should understand the normal functions of the healthy body. From the beginning, clinical content and basic sciences are taught in an integrated way in all modules. In the second and third year, the basics from the first year of study are taken up again. The modules are clinically oriented, but now turn more towards diseases and their therapy - based on the physiological basics learned in the first year. In the first three years of study, not only the "physics-relevant" subjects are taught in this way, but also to a large extent the basics of the clinical subjects. After three years, students complete their equivalent of the first part of the medical examination (M1). In the fourth year, the practical component increases significantly once again and the building blocks of the first three years (clinical knowledge, communication, examination) are brought together. A total of 18 weeks of block practical training are completed in clinics; these are prepared by twelve weeks of lectures. In the Clinical Training Centre, clinical-practical skills are again intensively trained on simulators and phantoms. Communication training is deepened in the fourth year of study with simulators and the teaching content is specifically linked to clinical content. In the fifth year of study, another module with courses follows; in addition, students are in various block practicals for six weeks and write a research paper for 16 weeks. The study programme is completed with the practical year (PJ) in three tertials of 18 weeks each.
Practical orientation
In each module, one week is reserved for practical experience. This can be shadowing in general medical or other specialist outpatient practices, but also research placements or elective placements, in which students can choose which medical professional field they would like to explore.
Within the first three years of study, students spend a total of six weeks in outpatient practice placements as part of the integrated internships, four of which are in general medicine. In the fourth and fifth years of study, the students mainly gain practical experience in the clinical setting, in line with the contents in the curriculum. The majority of the practical phases are completed in cooperation institutions of the University of Oldenburg (teaching practices, university hospitals and academic teaching hospitals). This ensures a uniform supervision concept and high-quality supervision, which contributes significantly to the students' learning progress.
- Simulation persons
- Events at the KTZ
- Communication and counselling
- Patient colleges
- POL
Competence-based study
A central objective of the model study programme is to train students in all the competences required in the medical profession and to prepare them for the future profession from the very beginning through patient-oriented studies. The curriculum is based on the national competence-based learning objectives catalogue for medicine (NKLM). The NKLM explains the professional roles of doctors (MFT (Medizinischer Fakultätentag der Bundesrepublik Deutschland e.V.) (ed.) (2015), Nationaler Kompetenzbasierter Lernzielkatalog Medizin. Leading up to this, the NKLM describes knowledge, skills, abilities and competences that are to be acquired in the course of studies. Depending on the level of education, different levels of competence are identified. Competences generally describe an interaction of available cognitive abilities, practical skills and attitudes in a person. Competences can be learned individually in order to be applied responsibly in different situations to solve problems.
In the medical field, the description of competence refers to the professional, prudent and eventually habitual use of knowledge, practical skills, clinical reasoning, communication, emotions, values and reflections in daily practice for the benefit of both the patient as an individual and the whole community served. The professional roles assumed by physicians are derived from the professional world of physicians and the demands of society. The Canadian CanMEDS framework describes seven physician roles:
- Medical Expert
- Learner/teacher
- Collaborator/member of a team
- Patient representative/health advisor/health advocate
- Manager/responsible party
- Professional/professionalism
- Communicator/Communication
This concept is internationally widespread and has also gained acceptance in medical education. It has been included as an integral part of the NKLM. These roles, or the teaching of the necessary competences, are reflected in the curriculum and in the teaching formats of the Oldenburg model study programme and are also reflected in particular in the longitudinal pathways and in the implementation of the Entrustable Professional Activities in the block internship and in the PJ.
In the block internship and the internship year, the concept of Entrustable Professional Activities (EPAs for short) is used to transfer competence-based training into clinical practice. Following the graduate profile of the National Competence-Based Learning Objectives Catalogue for Medicine (NKLM), EPAs are defined via these points:
- They describe self-contained clinical activities that can be authentically found in the medical field of work.
- They describe activities that are entrusted to students.
- They define and integrate the knowledge, skills, attitudes and competences relevant to these activities.
- They define the minimum requirements for students that are necessary for the safe and effective performance of an activity under a defined level of supervision.
The EPA concept is based on the gradual learning of medical-professional activities, which are transferred and entrusted to the students with increasing degrees of independence. The basis for this entrustment is:
- the sufficiently acquired competence to carry out the activity safely and effectively (= correctly) in terms of the result,
- the reliability and trustworthiness in the execution of the medical activity,
- as well as the ability to act within one's own limits, i.e. to seek help when assigned tasks prove to be too difficult.